What you need to know about Ulcerative Colitis?
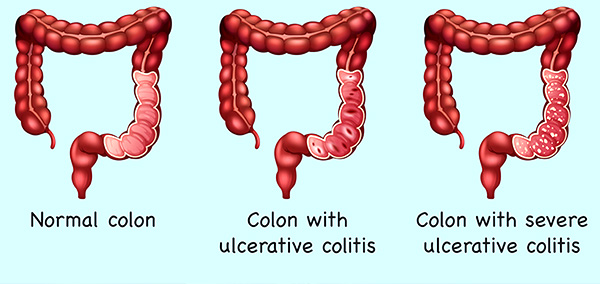
Ulcerative colitis is a disease of large intestine or colon. It’s an inflammatory condition which results typically in intestinal complaints of blood in motions and loose motions(diarrhoea), rectal pain, Urgency to defecate, abdominal pain, weight loss and fatigue. The patients also may experience symptoms like arthritis(Joint swelling and pain), skin related problems, Clotting of the arteries and veins, eye symptoms, jaundice in addition to bloody diarrhoea. Intestinal symptoms are way more common than the extra intestinal ones.
Is Ulcerative Colitis a Chronic disease?
Yes its is a chronic life long condition and it can be maintained in a symptom free state by medications/Surgery, though surgical treatment is required in rare situations. There is no cure discovered so far.
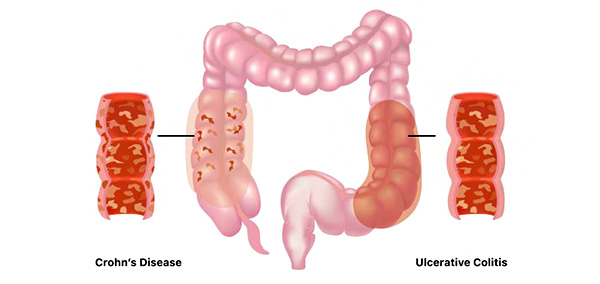
Does Ulcerative colitis run in families?
Yes, the likelihood of acquiring the disease is more often if one has a family member affected by Ulcerative colitis or Crohn’s disease.
How is Ulcerative colitis diagnosed?
- Stool routine microscopy
- Stool Calprotectin levels
- Colonoscopy and biopsy from inflammed areas.
- Rarely a CT scan/X ray may be ordered by your doctor if the disease is very severe.
- Hemoglobin may be low with an elevated ESR and low albumin if the disease activity is severe.
Living with Ulcerative colitis:
There symptoms of ulcerative colitis will come and go intermittently. The symptom free period is called remissions and the symptomatic period is called exacerbations. The number of exacerbations(relapse/symptomatic period) can be lessened by proper maintenance treatment and relapse can be shortened with prompt treatment at the onset of it. It’s a chronic and in curable disease.
Ulcerative colitis is very unpredictable disease making it difficult for both patients and doctors to predict the relapse of the disease even when the patient is on maintenance treatment.
How the Ulcerative colitis is monitored?
- Calprotectin levels in stool
- Colonoscopy
- Biopsy findings on Colonoscopy
How is Ulcerative colitis treated?
Medical therapy is the main stay of treatment- Medications include tablets 5 Aminosalycilate, Steroids, Azathiprine, Tofacitinib, Infliximab like agents. At times, if the disease activity and severity is limited, your doctor may advise only a suppository or enema of 5 Aminosalycilate or steroid.
When is surgery required in Ulcerative Colitis?
Surgery is required in severe cases when the disease activity is not controlled with medications, or for a colonic perforation or Toxic mega colon. Typically whole of colon and rectum are removed. Even after the surgery patient may continue to have extra intestinal symptoms of ulcerative colitis as mentioned.
Possible complications of Ulcerative colitis:
- Severe dehydration and bleeding
- Anemia
- Toxic mega colon- Transmural thickening and inflammation of colon
- Colonic perforation- Hole formation in colon
- Inflammation in eyes, skin, joints
- Increased risk of colonic cancer
- Osteoporosis- Bones getting weakened can lead on to fractures
What are the mistakes usually done by Ulcerative colitis patients?
- Not following up regularly with the gastroenterologist
- Not following the medications and trying out some form of homeopathy or ayurveda or alternative medications
- Not undergoing regular tests
- Patient may start to assume that since disease is under control, It’s not required to visit the doctor anymore(Remember disease is chronic and the disease can become active at any time even if the medication is being consumed by the patient).
Can you become pregnant with Ulcerative colitis?
It’s best to opt to become pregnant when the disease is fully under control. The medications are very safe during pregnancy. Medications of Ulcerative colitis if discontinued during pregnancy can result in disease becoming severely active and losing the pregnancy.
Diet and Ulcerative colitis:
No dietary restrictions are helpful except for milk and milk products when the disease activity is severe.
- Ultra processed foods are to be avoided at all times.
- Low salt diet advised when the patients is on corticosteroids
- Low fibre diet in disease active period to reduce bowel movements
- Certain vitamins and minerals become deficient in Ulcerative colitis patient B12, Vitamin C, Folic acid, Vitamin D, Iron, calcium, Zinc and magnesium.
- High calorie diet if the disease is very active or in those experiencing weight loss or growth delay.
Stress, emotional factors and Support in Ulcerative colitis:
Stress can contribute to disease severity. It’s best to avoid it at all times of the disease. There is no direct evidence to say that stress causes ulcerative colitis. Depression and mood instabilities are often found with all chronic diseases a mental health professionals help will go a long way in managing the disease holistically.